Laparoscopic Nissen Fundoplication
Description
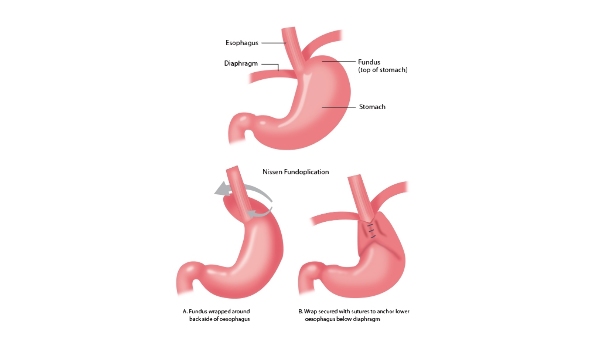
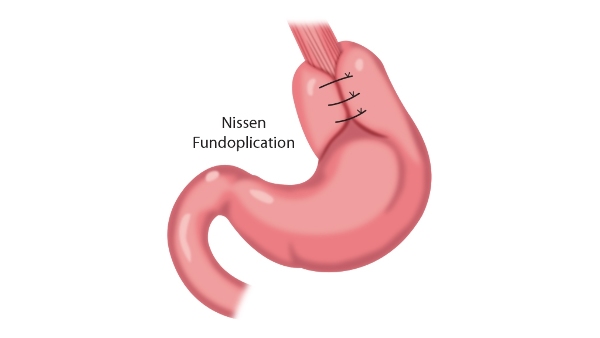
Laparoscopic Nissen Fundoplication is a minimally invasive surgical procedure used for the treatment of hiatus hernia and gastroesophageal reflux disease. It involves the wrapping of the top part of the stomach around the distal end of the oesophagus with the intention of strengthening the lower esophageal structures and preventing reflux. It is typically performed after standard medical treatment has failed to help.
The surgery is performed under general anaesthetic and recovery usually takes between 4-6 weeks, during which time the patient is advised to stay on a soft diet to prevent any damage to the newly formed wrap.
Common complaints after the procedure include dysphagia and bloating, which are usually transient but can persist, alongside more serious complications such as pneumothorax and esophageal perforation although these are rare.
What is it?
A Laparoscopic Nissen Fundoplication is a minimally invasive surgical procedure used in the treatment of gastroesophageal reflux disease and hiatus hernia. The surgical procedure involves two main goals:
- Strengthening of the weakened muscle of the esophageal hiatus, which is an opening in the diaphragm where the oesophagus passes down from the chest into the abdomen. This reduces the chance of recurrence of a hiatus hernia after the operation.
- Wrapping the top part of the stomach around the distal (lower) end of the oesophagus to strengthen the lower esophageal sphincter mechanism and help reduce reflux of stomach contents back into the oesophagus (1).
Why is it done?
The surgery is predominantly conducted to treat patients with gastroesophageal reflux disease and a hiatus hernia where previous medical treatment and lifestyle treatment has failed to alleviate the symptoms. Gastroesophageal reflux disease and hiatus hernia are two separate conditions and may occur by themselves, however it is common for these two conditions to be associated with one another.
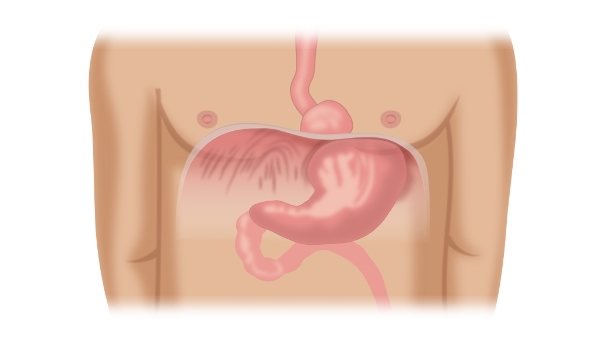
An opening called the esophageal hiatus exists in the diaphragm, which allows the oesophagus to pass from the chest into the abdomen. When this opening widens, it can result in a hiatus hernia where part of the stomach enters into the chest cavity (mediastinum).
While this is fairly common and symptomatic in
many people, it can also result in further complications such as
gastroesophageal reflux disease (GORD). This is where food or stomach acid
leaks back from the stomach into the oesophagus, resulting in irritation,
cough, and chest pain (heartburn).
There are a variety of treatments that should be tried before progressing to a Nissen Fundoplication. These include proton pump inhibitors, antacids, and lifestyle changes such as weight reduction and elimination of fizzy drinks from the diet. If you have tried all these approaches and the disease is still not getting better, your doctor will talk to you about the possibility of a Nissen Fundoplication (2). Generally speaking, for a patient to be considered for anti-reflux surgery such as a Nissen Fundoplication, their symptoms would be severe and may be associated with any of the following:
- History of aspiration pneumonia caused by food entering the oesophagus from the stomach, and then being aspirated into the lungs.
- Barrett’s Oesophagus
- Where the patient is unable to take medications either due to compliance issues or side effects that make taking them not viable or safe (3).
Anaesthesia
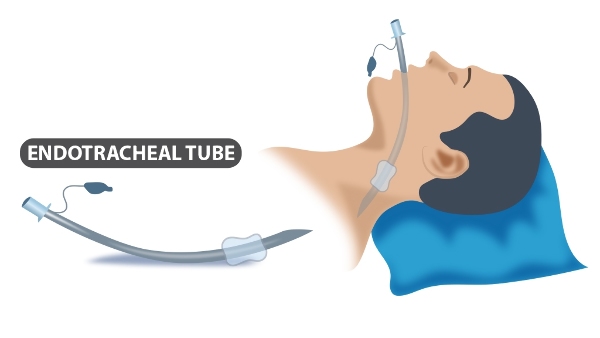
The surgery is carried out under general anaesthetic, which means that you will be unconscious throughout the surgery. For this reason, you will need to have an endotracheal tube placed down your throat to help you breathe during the procedure (see diagram below). You will have an appointment with the anaesthetist before the surgery where you can discuss any concerns or queries you may have, and go through any on the day procedures.
Will I need to do any preparation?
Before your operation, you will be seen in the preoperative clinic with your surgeon who will ask you some questions about your general health and conduct basic tests to ensure you are fit enough for the surgery to go ahead. The surgeon may order additional tests to confirm the diagnosis and to inform the approach required in the surgery. These tests include:
- Esophagogastroduodenoscopy (OGD) - This is an endoscopic procedure conducted in all GORD and Hiatus Hernia patients who are candidates for surgery. It involves inserting a thin tube with a camera into your mouth and then down your oesophagus. This allows the surgeon to assess for any other diseases within the oesophagus such as oesophagitis, as well as to test the patency of the gastroesophageal junction flap allowing entry of food contents into the stomach (6).
- Barium Esophagram - This procedure involves swallowing a special contrast solution while having a special scan conducted at the same time. This allows the surgeon to visualise any problems with the swallowing mechanism, alongside checking for any hiatus hernia.
- Esophageal Manometry - This is used to test the motility and peristalsis functions of the oesophagus, alongside testing the function of the lower esophageal sphincter. This procedure is useful in patients who require further investigations to exclude other causes of dysphagia (difficulty swallowing) such as achalasia.
The Surgery
The surgery takes between 60 and 90 minutes, and approximately 30 minutes before the surgery is expected to start you will be given a course of preoperative antibiotics to reduce the chance of infection occurring during the procedure. You will also be given a pair of compression stockings to wear which will help prevent blood clots from forming in the legs during surgery (Deep Vein Thrombosis).
There are a variety of different methods for conducting a laparoscopic Nissen Fundoplication, and exact procedures will differ from surgeon to surgeon. An example of the steps of the procedure are as follows:
- After being administered the general anaesthetic, an orogastric tube will be placed inside your stomach. This will allow for any removal of stomach contents to reduce the risk of aspiration pneumonia occurring during the surgery. You will be placed in the lithotomy position (see picture below). This will allow the surgeon the best possible exposure to conduct the surgery. The skin between your nipples down to the top of your groin area will be cleaned with a special cleaning solution to reduce the risk of any wound infection.
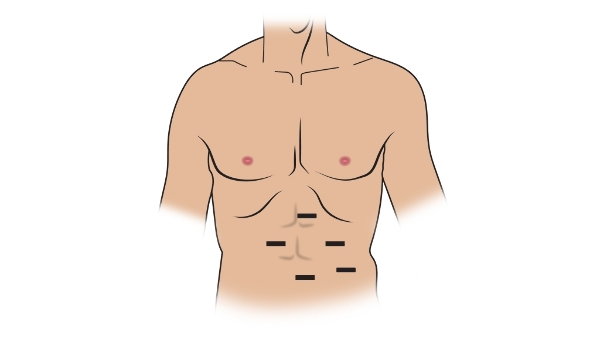
- Once in the correct position, the surgeon will make between 4-5 incisions in your abdomen for the various pieces of equipment to enter. These include a laparoscope, which is a thin tube with a camera on the end which allows the surgeon to see inside your abdomen using a TV screen. At this point, gas will be pumped into your abdomen to inflate it and give more room for the surgeon to work in. The common sites for incision include:
- Near the umbilicus (belly-button)
- Two incisions underneath your right rib
- Underneath your left rib
- Once the incisions have been made, you will be placed in the steep reverse Trendelenburg position for the surgery to begin.
- The surgeon will begin on the left hand side of the diaphragm. The first step in the surgery involves dividing the short gastric vessels. First the ligament that connects the diaphragm to the stomach (phreno gastric ligament) is divided, and the short gastric vessels which supply the greater curvature of the stomach are exposed. These vessels are then divided, and the left crus of the diaphragm can now be seen.
- The surgeon then turns their attention to the right side of the body, and starts by dividing the ligament that connects the stomach to the liver (gastrohepatic ligament). At this point, the surgeon has to take cure to ensure that any aberrant (not usually there) left hepatic artery is not mistakenly divided, which can result in liver complications if this occurs. A window is made behind the oesophagus, and the surgeon takes care not to damage the left and right vagus nerves that are closely associated with the oesophagus. Damage to these nerves can result in gastro-intestinal complications.
- The surgeon then begins to mobilise the oesophagus, starting with the distal (lower) end. In cases of hiatus hernia, there may be adhesions which join the oesophagus to the posterior abdominal wall. If these are present, they will be divided to allow the oesophagus to be fully mobilised. Once all the adhesions are divided, the surgeon will ensure that there is sufficient oesophagus present within the abdominal cavity, usually up to at least 3cm.
- The orogastric tube that was previously in place is now replaced with a French Bougie, which is a cylindrical instrument inserted into the stomach. The surgeon begins preparations for the wrap by marking out the areas which require to be stitched.
- The surgeon begins creating the wrap by passing the posterior fundus of the stomach from left to right, and the anterior fundus is then brought in front of the esophagus to join the posterior fundus. 3-4 sutures are placed to join the structures and oesophagus together.
- The French Bougie is removed, and the wrap is anchored to the diaphragm in 3 different positions.
- At this point, the surgery is now complete and the surgeon will inspect the area for any bleeding, and will then close the wounds using sutures (1).
Post-Operation
After the surgery has finished, you will be taken to a recovery room where you will be woken up. Your vital signs will be monitored and your wound sites inspected to ensure there is no infection. Once you are stable, you will be taken to a ward where you will stay for 2-3 days to recover before being discharged. During this time, your recovery will be closely monitored by the medical team, and pain relief will be available to help with any postoperative pain. You can start to eat a liquid diet, progressing to a soft diet as you see fit.
Caring for yourself at home
A soft diet is encouraged for up to 6 weeks after the surgery; hence it is recommended that you cut or blend up your food during this time period. Failure to do so may lead to the solid pieces of food becoming dislodged and unable to enter the stomach, which can impair the healing process. Before being discharged, a dietician will meet with you to discuss the different food options and to give you tips for ensuring you stick to a soft diet.
You can begin to drive again after about 10 days, and you can begin working again after 3 weeks as you see fit. It is important to avoid any heavy lifting or straining for up to 6 weeks after your surgery to ensure a good recovery and effective wound healing. After 6 weeks, you will have a follow up appointment with the surgeon who will check up on your recovery progress. This is a good opportunity for you to ask any questions or raise any concerns you may have.
You can continue to take painkillers during your recovery period to help with any postoperative pain, however if you notice any severe pain or fever it is important that you seek urgent medical attention as this may indicate a serious infection.
After discharge, a feeling of bloating is common, occurring in between 11% - 40% of patients (7). This is often transient and goes away over time. If this persists, the doctor may prescribe you with some simethicone or charcoal caplets, alongside some recommendations for lifestyle changes such as the avoidance of fizzy drinks and caffeine. In severe cases, botox injections or pyloric dilatation procedures can be trialled to help alleviate the bloating (8).
Where can I find more information
NHS information on reflux disease - https://www.nhs.uk/conditions/heartburn-and-acid-reflux/
NHS information on hiatus hernia - https://www.nhs.uk/conditions/hiatus-hernia/
Comments