Hemorrhoid banding
Hemorrhoid banding
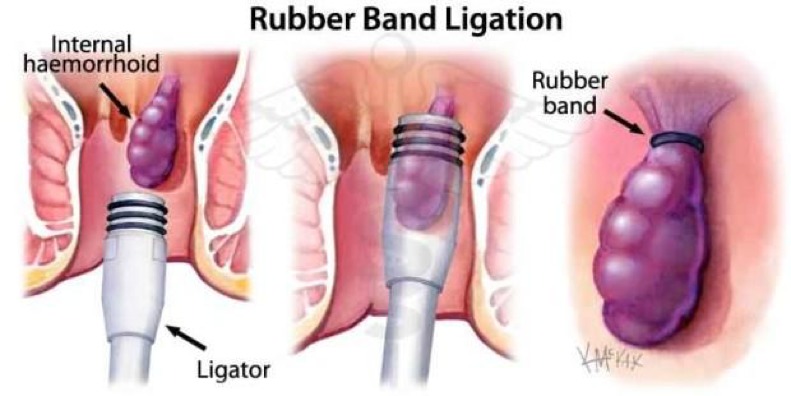
Rubber band ligation is a procedure involving the placement of rubber bands on internal hemorrhoids which are not responsive to home and topical based remedies. The procedure is not performed on external hemorrhoids, alongside those with coagulation disorders due to the risk of bleeding. The placement of the rubber band constricts blood supply to the hemorrhoid and causes it to fall off over time.
Due to the relatively quick and simple nature of the procedure, no anesthesia is used unless several hemorrhoids need to be banded in one session. Recovery usually involves pain management using standard pain medication such as paracetamol, and bed rest for 2-3 days after the procedure. Particular emphasis is placed on dietary modifications and increased fluid intake to avoid straining when defecating in order to prevent recurrence of hemorrhoids.
Complications of the procedure range from pain which is relatively common, to more severe complications such as infection and delayed hemorrhage resulting from misplacement of the rubber band.
Hemorrhoid band ligation is the most commonly used treatment for treating symptomatic internal hemorrhoids due to its simplicity, low cost, and low risk for complications. The procedure involves tying off the base of the hemorrhoid with rubber bands, effectively cutting off blood supply to it and causing it to necrose and fall off over time (1).
The procedure is only performed on internal hemorrhoids, and hence external hemorrhoids are not treated in this way. Hemorrhoids are typically benign and can usually be left alone. Treatment is only indicated if you feel as if your symptoms are severe enough. Hemorrhoids are usually treated using home remedies and topical creams. If the internal hemorrhoids do not respond to this treatment, they can become increasingly itchy and painful and hence rubber band ligation may be recommended (2).
Rubber band ligation is often considered to be the most effective non-surgical treatment for internal hemorrhoids. While surgical removal of hemorrhoids through hemorrhoidectomy may provide better long-term results and success rates for recurrence, it is more expensive, results in longer recovery times, and has a greater risk of complications. Rubber band ligation is also more readily available whereas surgical hemorrhoidectomy requires surgeons who have been specifically trained in that procedure. If there is any recurrence of hemorrhoids after rubber band ligation, further procedures can be easily scheduled to take place (3).
Before the procedure, the doctor will evaluate the medications you are currently taking to see if rubber band ligation is a suitable procedure for you. If you are taking anticoagulant medication such as warfarin and clopidogrel, or if you have certain coagulopathies (blood clotting disorders), then rubber band ligation may be contraindicated for you and hence the doctor will discuss alternative approaches. This is due to the risk of delayed bleeding (4).
Standard hemorrhoid band ligation does not require any local or general anesthesia, however sedation may be given to reduce discomfort and help you relax during the procedure. Please speak to the nurse or doctor before the procedure takes place if you would like to request a sedative, as they will have to go through some safety procedures with you to ensure you are not allergic to the sedative.
In more severe cases of internal hemorrhoids where there are several hemorrhoids that need to be banded, general anesthetic can be used to mitigate the pain and discomfort. However this is relatively rare and if several henmorrhoids need to be banded, it is more common for the doctor to schedule multiple rubber band ligation appointments with sufficient time in between to ensure the area has healed.
The procedure is usually conducted as an outpatient procedure and hence you will not need to stay overnight in hospital as long as there are no complications. The whole procedure is short and is usually completed within 20 minutes. If there are 2-3 hemorrhoids present, then they can all be banded in one session as long as you are comfortable and can tolerate it. On arrival at the department, a member of the nursing team will conduct an initial assessment and you will be provided with a consent form and a gown to change into. The procedure is as follows:
1) You will be placed in either the semi-inverted jackknife or left lateral position. You will be given pillows to help you feel more comfortable.
2) An anoscope (a viewing instrument) is inserted into the anus, allowing the doctor to visualise the hemorrhoids.
3) The doctors will identify the largest hemorrhoid first and hold it with forceps.
4) The trigger on the end of the rubber ring ligating drum will cause rubber bands to be released onto the hemorrhoid.
5) At this point, you will be asked about any pain to assess whether the rubber band has been placed in the correct position.
Once the rubber bands have been assessed to be correctly fitted, the equipment will be removed and the area cleaned. In the next 3-5 days after discharge, the rubber band will cause the hemorrhoid to thrombose and become ischemic. Eventually, the hemorrhoid shrinks and falls off, resulting in damaged tissue which takes several weeks to fully recover (5).
The whole procedure is short and is usually completed within 20 minutes.
Since rubber band ligation is an outpatient procedure, you will be allowed to go back home once the procedure is done. Usually, between 1-2 hemorrhoids can be banded in any given session provided that general anesthetic is not used. Hence if you have hemorrhoids remaining that have not been banded, you will need to have the procedure repeated and will be given a follow up appointment after 6-8 weeks to ensure that tissue from the original procedure has healed properly.
It is recommended to try not open your bowels until the day after your banding, however this may not always be possible.
This is almost always a day case procedure.
After discharge, the doctor will recommend you to return to normal activities as you see fit. Most people may require 2-3 days of bed rest to allow for the pain to fully subside. Standard pain relief such as Paracetamol can be used to reduce the pain, alongside warm baths with sitz salts. If you take aspirin and any NSAIDs, the doctor will advise you to avoid taking these in the few days before and after your operation to reduce the risks of any delayed bleeding. The hemorrhoid is likely to fall off between 7-10 days after surgery, and hence a small amount of bleeding may occur at this stage; although this is minor and likely to stop by itself.
This is rarely necessary.
The doctor will advise you on any dietary and behavioural changes required to be taken to reduce the risk of hemorrhoid recurrence. These include taking stool softeners and ensuring plenty of fibre and fluid intake to prevent straining when defecating, which increases the likelihood of hemorrhoid formation (6).
This is dependent on the findings and the doctor will advice you.
Usually the next day but will dependent the number of haemorrhoids treated and the nature of the activity.
Comments