Type 1 Diabetes Mellitus (T1DM)
What is type 1 diabetes?
Type 1 Diabetes Mellitus (T1DM), also known simply as type 1 diabetes, is life-long condition affecting the bodies’ ability to control the level of blood sugar. If not controlled, this can affect various part of your bodies, such as your eyes, your kidneys and nerves and put you at greater risk of getting heart attacks and strokes. In type 1 diabetes, your pancreas are damaged by the body’s own immune system and therefore don’t produce any insulin.
The pancreas is an organ in the human body that produces various hormones, or in other words, chemical messengers, that are released and circulate around the body and communicate with other organs and muscles to carry out functions. One such hormone the pancreas produces is insulin, which allows the body to control the level of the blood sugar. The level of sugar in a person’s blood is tightly regulated to make sure the body can undertake everyday functions and also avoid the damaging effects of high blood sugar. In type 1 diabetes, the pancreas is damaged by the bodies’ own immune system.

The result of this is that the pancreas can no longer produce enough insulin to control the blood sugar level. This leads to long-standing increase in blood sugar levels which increases the risk of developing cardiovascular disease and can directly damage the blood vessels and nerves, in particular, those supplying the kidneys and eyes (see Complications).

Insulin also allows the body to use the sugar in blood, without it there is reduced uptake of sugar intake the organs and muscles. Additionally, the absence of insulin in the blood stream triggers the body to enter starvation mode and means that the body starts to produce an energy substitute known as ketones. If these ketones accumulate in the presence of dehydration this can be dangerous (see Complications).
What causes type 1 diabetes?
The number of people developing type 1 diabetes has increased over the last 30 years. Type 1 diabetes is caused by the immune system, designed for fighting infections, attacking the cells in the pancreas itself.
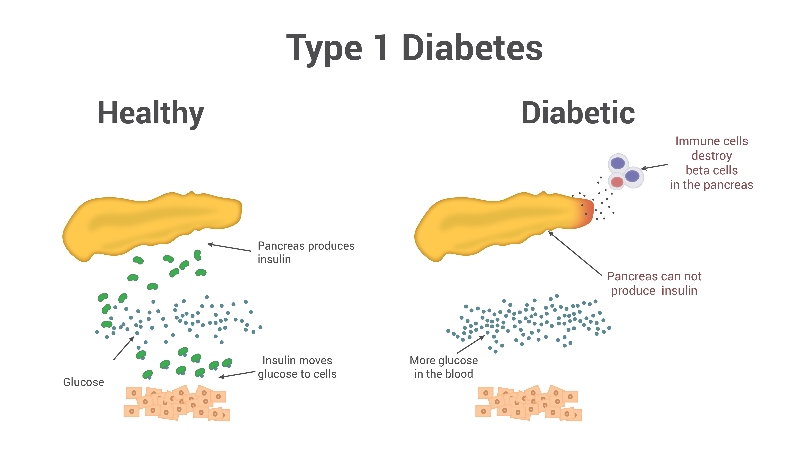
This is known as auto-immune (meaning the immune system attacking part of the body) mediated destruction. We know this is the case as the majority of people with type 1 diabetes have detectable antibodies (immune cells) in their blood that specifically target parts of the pancreatic make up. The pancreas is an organ in the human body that produces various hormones in the body. One such hormone produced by the pancreas is Insulin and it is produced by cells in the pancreas called beta cells. The cells in the pancreas that produce insulin are known as beta cells. These cells are gradually depleted or destroyed until there is no longer enough insulin to control the blood sugar level.

When considering what causes a disease, there is an interplay between someone’s genetics and what they are exposed to in life. The genetic code involved writes the script for the molecules that present bugs and infections to the immune system. People with type 1 diabetes have part of genetic code that writes script for antibodies that target parts of their own pancreas. Some of the environmental factors and key exposures thought to be involved in the development of type 1 diabetes include certain viruses (enteroviruses) and dietary factors (vitamin D) – however the mechanism behind this is complex. Other risk factors include infections whilst in womb, infections as a young baby and dietary deficiencies as well as an increased body weight as a child.
What tests will I undergo to diagnose type 1 diabetes?
The diagnosis of type 1 diabetes is made on the grounds of a fitting picture of the condition alongside blood tests – the diagnosis is made by a specialist Endocrinologist.
The first investigation undertaken in the majority of people will be to test the level of blood glucose (sugar). This can be taken after a person has been instructed not to eat (fasting test) or in the form of a glucose tolerance which involves a blood test 2 hours after consuming a set amount of sugar in the form of a drink.
Another investigation is measuring a marker in your blood known as HbA1c can indicate the average level of blood glucose over 60 days and both helps in the diagnosis and monitoring of the condition.
The doctor might also measure the amount of known antibodies against antigens in the pancreas is commonplace with many people being tested for antibodies against glutamic acid decarboxylase, tyrosine-phosphate-like molecule or insulin.
Furthermore, the level of insulin in addition to a breakdown molecule of insulin known as c-peptide can also help to diagnose diabetes. If these antibodies are present, it supports the diagnosis of diabetes. However, their absence does not rule out diabetes and a person can still be diagnosed with type 1 diabetes.
Epidemiology
Type 1 diabetes accounts for up to 10% of all causes of diabetes. The most common time for developing (or diagnosing) type 1 diabetes is around 5 – 14 years of age and it is the most common type of diabetes seen in young people. It is slightly more common in males in comparison to females. The number of people with type 1 diabetes varies around the world for example, it affects 60 per 100,000 people in Finland whilst as few as 0.1 per 100,000 people in India, China or Venezuela. In the UK type 1 diabetes affects around 400,000 people. Generally, the number of people developing type 1 diabetes is generally increasing across the world and it is thought to affect over 1 million people worldwide.





Comments