Laparoscopic Left Hemicolectomy
Laparoscopic Left Hemicolectomy
Laparoscopic Left Hemicolectomy is a minimally invasive surgical procedure involving the removal of the left side of the colon which may also include the sigmoid and rectal regions. It is typically performed in cases of left sided bowel cancer, alongside less common reasons such as inflammatory bowel disease and cecal volvulus.
The surgical procedure is performed under general anaesthetic and recovery takes up to 6 weeks. During the recovery period, the patient is encouraged to keep active and maintain an adequate fluid and fibre intake. Postoperative pain can be managed using over the counter pain medication.
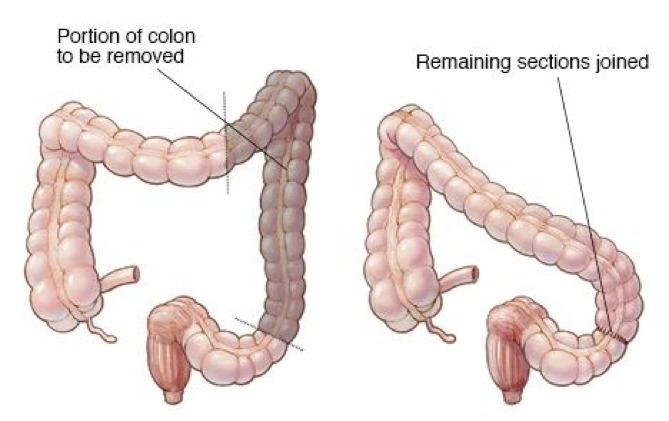
A laparoscopic left hemicolectomy is a minimally invasive surgical procedure involving the removal of the left side of the colon, alongside forming an anastomosis (attachment) of the end of the transverse colon with the rectum. The colon is split into a right and left portion, with the left side consisting of the descending and sigmoid colon, alongside its associated vascular pedicles (1).
There are many reasons why a laparoscopic left hemicolectomy needs to be performed. These include: - Colon cancer - This is the most common reason necessitating removal of the left colon. The cancer may either be primary and originated within the bowel, or may have spread there from elsewhere in the body (metastasis). - Diverticulitis - Diverticular disease refers to the formation of outpouchings in the wall of the colon, particularly in the sigmoid region of the left colon. While diverticular disease is in fact very common, especially among elderly people, a complication called diverticulitis can develop, where there is severe inflammation of these areas. Where there is chronic diverticular disease, or severe acute diverticulitis that is refractory to medical treatment, surgical removal of the affected part of the colon may be necessary (2). - Colonic Polyps - The presence of a polyp may also necessitate removal of the left colon if the polyp has a high malignant potential, that is to say it has a high probability of becoming cancerous. Hence this is done as a preventative procedure (3). - Ischaemic Colitis - This occurs when blood supply to the colon is restricted, resulting in inflammation and injury. If left untreated it can progress onto bowel ischaemia (4). - Inflammatory Bowel Disease - This includes conditions such as Crohn's Disease and Ulcerative Colitis, where the colon becomes inflamed and in severe cases requires removal. In the case of ulcerative colitis, removal of the affected portion of the colon can be a curative treatment (5).
Laparoscopic left hemicolectomy has been shown to result in quicker recovery times and lower complication rates including bleeding and wound infection than the equivalent open procedure due to its minimally invasive technique (6).
You will be required to attend a pre-admission clinic with the surgeon and anaesthetist approximately 2 weeks before the operation is scheduled to take place. Here, your vital signs will be measured and you will be given information about the procedure and what to expect. This is also a good opportunity to ask any questions or raise any concerns you may have. It is important that you bring your medications with you as certain medications such as anticoagulants may need to be temporarily stopped in the period before your operation to reduce the risk of complications.
If you haven’t had one already, the doctors may send you off for imaging of your bowel to locate the tumour via a CT-scan. This will help the doctors assess which portion of the bowel needs to be removed and if the transverse colon should be removed alongside the caecum and ascending colon. You may also have blood tests and an ECG conducted to check for any other issues that may need correcting before the surgery occurs and to ensure you are fit enough for the major surgery to proceed.
There are a variety of different preparations that may need to be conducted to help prepare your bowel for the operation. These include:
- Following a special diet in the few days before your operation, including a balance of fruit and vegetables.
- Taking laxatives or enemas before your operation to ensure any bowel contents are removed and hence the colon is empty and ready for surgical removal.
- Taking of supplements to correct vitamin and electrolyte imbalances
- If you smoke, you will be strongly encouraged to stop smoking before the operation as this will greatly increase the chances of a successful recovery.
In order to prevent the risk of any complications, particularly aspiration, you will be asked to stop eating 6 hours before the surgery is scheduled to take place, and to stop drinking 2 hours before the surgery.
Before the anaesthetic is given, you will likely be administered a course of prophylactic antibiotics to prevent the risk of infection. These include cefuroxime and metronidazole, which have been shown to reduce the risk of sepsis occurring during removals of the colon.
The procedure is formed under General Anaesthetic and typically lasts between 3-4 hours. On the day of your operation, you will meet the Anesthetist who will go through the procedure and discuss any concerns or questions you may have. Because general anaesthetic will be used, you will be unconscious throughout the surgery. As a result, an endotracheal tube will need to be placed down your throat to help you breathe.
The whole procedure will take between 2-4 hours. The steps of the procedure are as follows:
- Once the general anaesthetic has been given, you will be placed in the supine position, with your legs split (see diagram below). The abdomen will be sterilised using a chlorhexidine preparation to minimise the risk of any infections developing at the incision site.
- Incisions will be made in the abdomen for the various different pieces of equipment to enter. These include the laparoscope, which is a thin tube with a camera on the end, allowing the surgeon to visualise and perform the operation. Incisions will typically be made at the following sites:
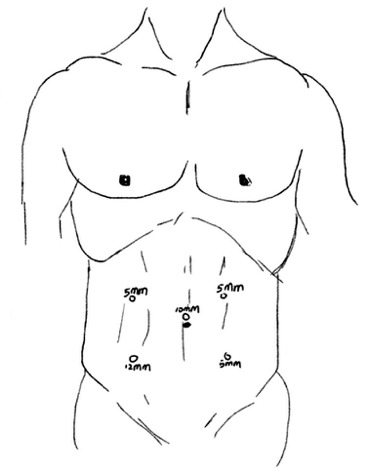
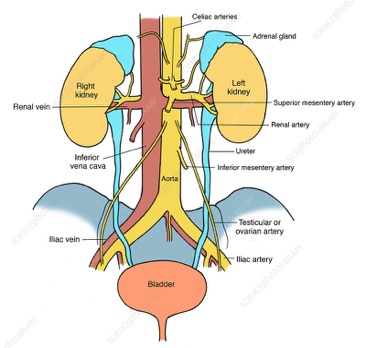
- Once the incisions have been made; the equipment is inserted into the abdomen. Gas may be pumped into the abdomen to inflate it and allo the structures to be more easily visualised by the surgeon. The surgeon starts by exploring the abdomen using the laparoscope to identify if there has been any metastasis to nearby organs. The surgeon begins the operation by mobilising the sigmoid colon, taking a medial to lateral approach. The sigmoid mesentery that connects the sigmoid colon to the pelvic wall is first divided, which reveals the inferior mesenteric artery. The surgeon takes care not to damage the ureter which lies next to the inferior mesenteric artery. Damage to the ureter can result in abdominal pain and difficulty in passing urine. The inferior mesenteric artery is divided close to its junction with the abdominal aorta as this artery supplies the left part of the colon with its blood suppThe descending colon is then mobilised using either electro-cautery or ultrasonic dissection techniques until it reaches the splenic flexure. This involves removing any adhesions that the descending colon may have to the bowel wall. The surgeon then moves onto mobilising the splenic flexure. The first step involves transecting the gastrocolic ligament which stretches from the greater curvature of the stomach to the transverse colon. This allows the surgeon to enter an abdominal anatomical space known as the lesser sac. When dissecting this ligament, the surgeon takes care not to damage the splenic hilum, which carries the vessels supplying blood to and from the spleen. Damage to the splenic hilum and spleen can be serious and in severe cases requires a removal of the spleen (splenectomy) to treat. The surgeon takes care to preserve the marginal artery of Drummond (this connects the inferior mesenteric artery to the superior mesenteric artery) and the remaining branches of the middle colic artery (this supplies the transverse colon). Damage to these vessels can disrupt blood supply to the remaining portions of the colon. Once the surgeon has fully mobilised and dissected out the descending colon and splenic flexure, it is time for them to form an anastomosis (join) between the transverse colon and the rectum. This is done using an end to end anastomosis with staples to form a continuous passageway for disgusted food to enter the rectum and be excreted out of the body. The equipment is then removed, and gas is pumped into the abdomen once more to check the integrity of the anastomosis and ensure there is no bleeding in the operative field (7).
The whole procedure will take between 2-4 hours.
Once the surgery has been completed, you will be taken to a recovery room where you will be woken up and your vital signs monitored. You will be given some intravenous painkillers to help deal with the postoperative pain, and you may have a drainage tube in site where the operations took place to remove any accumulating fluid. After the anesthesia was administered, a urinary catheter would have been inserted to help drain the urine. This will have to remain in place for 1-2 days before it can be removed.
You can expect to stay in hospital between 4-8 days depending on your recovery. The medical team will regularly check up on you and inspect the wound sites to assess whether you are fit for discharge. During this time, you will be given water to drink, and eventually soft food when you feel more comfortable. You will also be encouraged to move and be active, as this helps recovery in the long term and reduces the risk of deep vein thrombosis (blood clot formation in the legs).
Full recovery may take between 4-6 weeks, and during this time you may feel weak and tired. Hence it is important that you have someone with you at home to help you with daily activities such as shopping and cleaning. For the first 6 weeks post discharge, avoid any heavy lifting and strenuous exercise.
As part of your recovery, it is important that you incorporate gentle exercise in your daily routine, as prolonged bed rest hinders your recovery from surgery and increases the risk of blood clot formation. An example of gentle exercise included walking in the garden. You may have more frequent and loose bowel motions than normal for the first few days after discharge, although this is expected to improve over time.
It is normal to feel pain and unusual sensations around the wound site and in your abdomen, even after several months. In most cases, this is due to healing and hence you can manage this using simple over the counter painkillers such as paracetamol to help you feel better. If the pain is severe and worsening over time, contact your doctor urgently as this may indicate an infection or leak.
Once discharged it is a good idea to have someone stay with you for one night if you live alone.
This is unlikely but will all be on a case by case basis.
This is again dependent on case and will all be explained by the doctor.
It is important to know that this is a major operation but because of the key hold nature it is common to be able to partake in your usual activities sooner. This varies between patients but usually a week is a rough estimate.
Comments